¶ Abstract
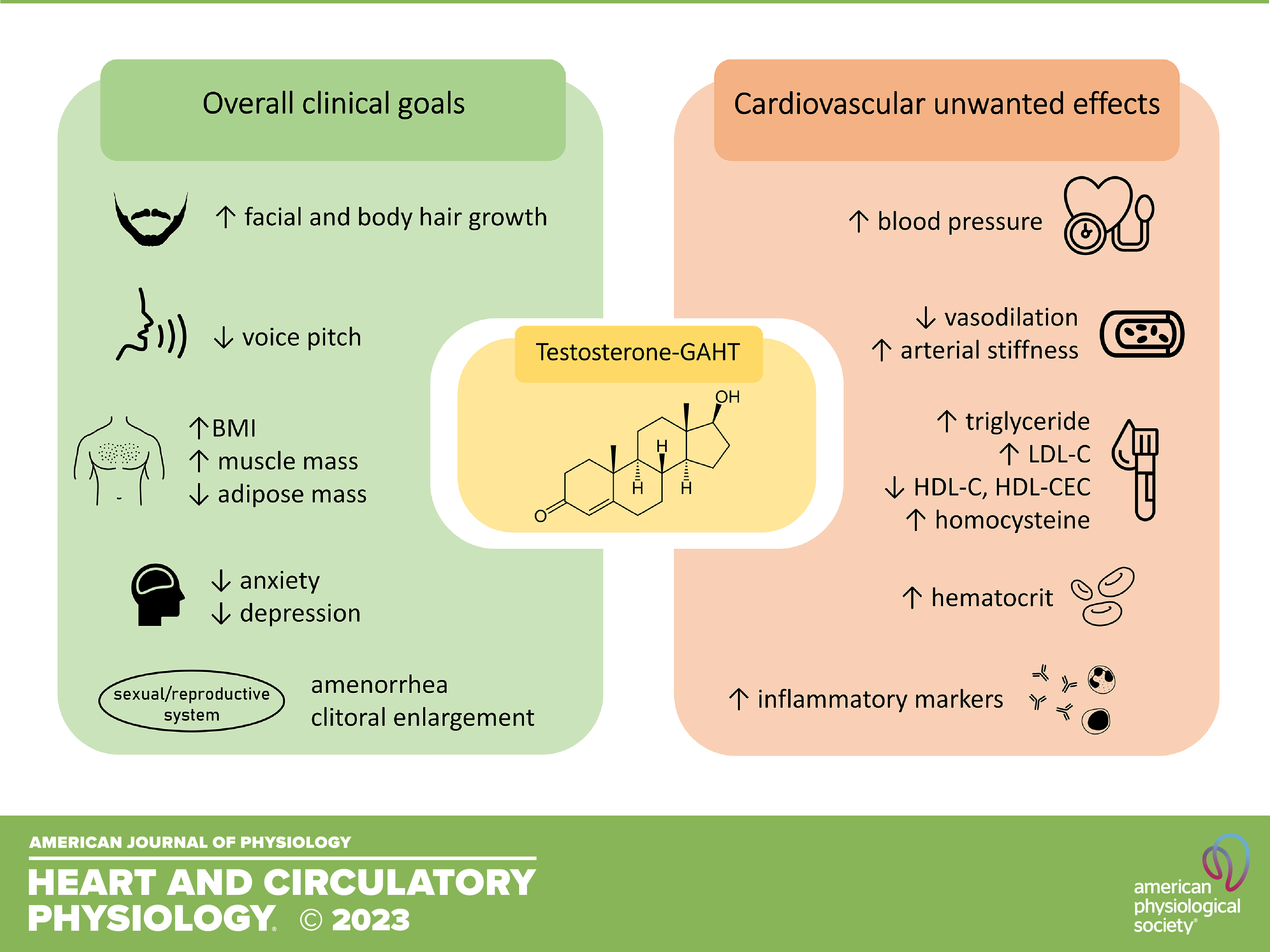
The growing number of people who identify themselves as transgender has gained increased attention in recent years and will certainly impact personalized clinical practices and healthcare worldwide. Transgender and gender non-conforming individuals frequently undergo gender-affirming hormone therapy (GAHT), i.e. they use sex hormones to align their gender identity with their biological characteristics. Testosterone is the main compound used in GAHT by transmasculine people, leading to the development of male secondary sexual characteristics in these individuals. However, sex hormones, testosterone included, also influence hemodynamic homeostasis, blood pressure, and cardiovascular performance by direct effects in the heart and blood vessels, and by modulating several mechanisms that control cardiovascular function. In pathological conditions and when used in supraphysiological concentrations, testosterone is associated with harmful cardiovascular effects, requiring close attention in its clinical use. The present review summarizes current knowledge on the cardiovascular impact of testosterone in biological females, focusing on aspects of testosterone use by transmasculine people (clinical goals, pharmaceutical formulations, and impact on the cardiovascular system). Potential mechanisms whereby testosterone may increase cardiovascular risk in these individuals are discussed, and the influence of testosterone on the main mechanisms that control blood pressure and that potentially lead to hypertension development and target-organ damage are also reviewed. Additionally, current experimental models, which are key to reveal testosterone mechanistic aspects and potential markers of cardiovascular injury, are reviewed. Finally, research limitations and the lack of data on cardiovascular health of transmasculine individuals are considered, and future directions for more appropriate clinical practices are highlighted.
¶ Conclusion And Clinical Perspectives
The worldwide population who identifies as transgender and seek healthcare services represents an important clinical demand. The cardiovascular impact of testosterone GAHT is debatable and still very preliminary. Reported harmful cardiovascular effects induced by testosterone GAHT include increased blood pressure, impaired vasodilation, arterial stiffness, dyslipidemia, maladaptive cardiac hypertrophy, and increased inflammatory markers. These events can potentially increase cardiovascular risk in those individuals and may significantly impact the healthcare system worldwide. In addition, unsupervised or indiscriminate use of testosterone by transmasculine people, especially in low- and middle-income countries, increases the risk of adverse events and can further impact the health system.Current clinical data assessing the cardiovascular effects of testosterone GAHT are mainly derived from cross-sectional studies, and data from longitudinal studies are missing. GAHT duration and starting age of individuals, the existence of cardiometabolic comorbidities, and sample size should be considered for more accurate evaluation. Preclinical studies addressing the cardiovascular effects induced by testosterone GAHT, especially studies aimed to investigate mechanisms that mediate testosterone effects, are essential to prevent or mitigate adverse events associated with testosterone GAHT. Preclinical studies should consider
1) pharmacological aspects such as the choice of the androgen, dose, route, volume, and
frequency of administration to closely mimic clinical use;
2) the induction of a “male” phenotype;
3) “defeminization” effects of the GAHT
4) starting age and duration of GAHT. Together, these aspects certainly will contribute to testosterone GAHT optimization, decreasing the cardiovascular
risk for transmasculine individuals.
¶ Links
Santos, J. D., Oliveira-Neto, J. T., & Tostes, R. C. (2023). The cardiovascular subtleties of testosterone on gender-affirming hormone therapy. American Journal of Physiology-Heart and Circulatory Physiology, 325(1), H30–H53. https://doi.org/10.1152/ajpheart.00015.2023
― 01 Jun 2023